Pain rests at the crossroads of physiology, psychology, and social context. A paramedic maintains a broken femur at 2 a.m., a registered nurse coaches a patient via the first 24-hour after stomach surgical procedure, a physio therapist reconstructs flexibility while juggling neuropathic discomfort flare‑ups. Each discipline sees a different face of the trouble, yet every one of them affect how much the individual experiences and exactly how rapid they recuperate. That is why targeted pain management training, from short courses to formal qualification, has actually become a core part of specialist advancement for allied health.
This overview outlines what to get out of a pain monitoring program, how qualification matches method for nurses, physiotherapists, paramedics, and various other clinicians, and how particular frameworks like PUAEME008 Offer discomfort administration shape day‑to‑day choices in emergency setups. It leans on actual scenarios, practical evaluation suggestions, and a frank take a look at trade‑offs you will meet in the field.
The case for organized discomfort education
Most medical professionals very first learn discomfort evaluation in a generalist program. You remember the 0 to 10 mathematical score scale, the Wong‑Baker deals with, and the essentials of NSAIDs versus opioids. Then fact complicates things. A mental deterioration patient that can't reveal requirements. A teen that looks great yet rates their pain at 9. A post‑op instance where you titrate morphine only to locate the pain is mostly spasm and anxiety. Without structured refresher courses, practices set in and nuance fades.
Modern pain management training courses are designed to shut that space. Good programs bring a biopsychosocial lens, sensible pharmacology, and abilities for severe and chronic contexts. They also upgrade you on security requirements and regulation, for instance real‑time prescription monitoring, local analgesic protocols, and non‑pharmacological complements that satisfy standard limits for evidence.
What counts as a quality discomfort management course
A credible discomfort monitoring certificate course balances theory and hands‑on practice. Seek evidence‑based educational programs, transparent learning results, and assessment that evaluates judgment instead of memorizing recall. When I assess a program for our group, I try to find 3 essentials. Initially, organized analysis training that goes beyond a solitary range and includes function‑based actions, warning screening, and review periods. Second, pharmacology that differentiates nociceptive, neuropathic, and combined pain, with clear dosing structures, titration techniques, and security tracking. Third, non‑drug strategies that are more than platitudes: led pacing, rated exposure, breathing or leisure methods, and device‑based options like TENS with functional parameters.

Accreditation matters, but the details vary by nation. Several pain monitoring training courses align to national competency frameworks or proceeding expert development (CPD) standards. In emergency situation contexts, discrete systems of proficiency like PUAEME008 Offer discomfort administration act as criteria for paramedics, occasion paramedics, and very first responders who need a firmly scoped capability for severe care.
Spotlight on PUAEME008 Supply discomfort management
PUAEME008 Offer pain administration is an unit of proficiency made use of in a number of Australian emergency situation treatment qualifications. While the wording can vary in training bundles, the significance is consistent: evaluate discomfort quickly, choose proper analgesia within extent and methods, administer safely, monitor response, and hand over properly. I first dealt with a team transitioning from an older device to PUAEME008, and the modification required cleaner documentation practices and more self-displined reassessment periods, which right away boosted client experience at sporting activities occasions and remote clinics.
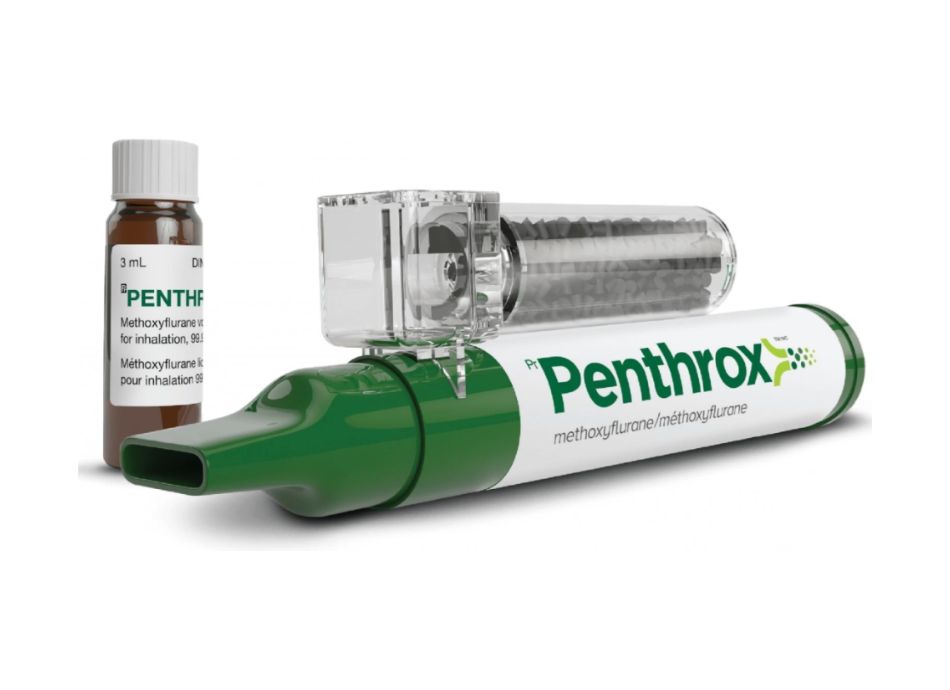
For medical professionals in these atmospheres, the strength of PUAEME008 is its operational quality. You discover specifically when and just how to deploy inhaled methoxyflurane for modest injury pain, when to rise to opioid analgesia within service guidelines, just how to use complements like splinting and cold therapy, and exactly how to track sedation and respiration making use of standard monitorings. The system also emphasizes spoken consent, contraindication screening, and rise to sophisticated care when discomfort is not responding as expected.
If your function consists of emergency discomfort monitoring in the area, a PUAEME008 give discomfort monitoring course can be the difference between improvisation and self-displined method. Employers commonly incorporate it right into onboarding for occasion clinical team, mine website medics, or remote location responders, then audit records against unit standards during annual abilities checks.
Matching programs to expert roles
Not every discomfort management certification offers the very same need. A healthcare facility nurse utilizes different levers than an area physio therapist, and a paramedic encounters one-of-a-kind time stress and scene hazards. Pick training that values your extent and context.
Nurses take advantage of pain management training courses for registered nurses that cover post‑operative pathways, PCA tool safety, opioid stewardship, ecstasy danger, and communication with family members that might merge sedation with comfort. Consist of modules on non‑verbal pain analysis for vital care, and on practical subjects like transforming opioid dosages throughout step‑downs from IV to dental routines. Paediatric nursing needs unique interest to weight‑based dosing and developing communication.
Physiotherapists look for pain monitoring courses for physiotherapists that mix pain neuroscience education and learning, graded task preparation, and methods for main sensitization without encouraging wonder remedies. A good program teaches you how to rate development when a customer oscillates in between flare and worry evasion, exactly how to incorporate rest and anxiety screening, and how to coordinate with prescribers when neuropathic attributes call for medicine modifications. Hands-on treatment and workout are still crucial, however the framework shifts from repairing tissues to constructing capacity.
Paramedics and first responders require short courses in pain monitoring that emphasize quick analysis, secure analgesic choice on the move, and useful complements like immobilization and disturbance. Inhalational choices, intranasal paths, and small‑volume devices matter when your patient is trapped in a vehicle or moving down a slim stairwell. The PUAEME008 give discomfort management framework is very pertinent here.
Allied wellness outside these classifications, such as occupational therapists, foot doctors, and radiographers, typically seek a certification course suffering administration to improve person preparation and adherence. As an example, radiographers that coach deep breathing and positioning can reduce motion pain throughout imaging and enhance research quality. OTs can teach power conservation and job simplification that lower pain burden without medical changes.
Core material you need to expect in a pain monitoring qualification course
Even as program titles differ, the core domain names are surprisingly constant when programs are built on existing proof. Anticipate a structured progression from mechanism to management.
Assessment basics. You ought to practice multiple ranges, discover when to choose each, and support scores to work. I encourage nurses to include 2 feature inquiries for any kind of admitted person: what movement activates discomfort most, and what does successful alleviation enable in the next six hours. Reassessment protocols are equally as vital as initial racking up. A solid training course needs paperwork of both peak discomfort and worst movement pain, given that these are typically different.
Pharmacology with guardrails. Pain administration training must distinguish nociceptive, neuropathic, and blended discussions, then link each to first‑line options. As an example, neuropathic pain often responds partly to gabapentinoids or SNRIs, while pure tissue injury may react far better to NSAIDs and paracetamol, with opioids reserved for brief windows. Titration methods, optimal daily doses, renal and hepatic adjustments, and medicine communications belong in the practical notes you actually keep at the bedside or in your kit.
Non medicinal methods with execution information. A lot of courses listing heat, ice, and TENS without parameters. Quality training spells out timing, regularity, and hints for stopping. It also resolves cognitive techniques like reframing pain signals throughout graded direct exposure, or how to use breathing patterns throughout wound care. For chronic pain, you want clear advice on sleep health training, flare‑up planning, and micro‑goals that construct a feeling of control.
Risk monitoring and opioid stewardship. Programs worth your time include product on opioid‑induced respiratory system depression, constipation prevention, and diversion danger. In 2020 our service lowered ED observation time for moderate trauma cases by approximately 15 percent after re-training personnel in a simple titration and review cycle for IV morphine, coupled with set up laxatives and a handover script. The mechanics are teachable, and they pay off.
Communication with clients and families. The best discomfort administration training for registered nurses and physiotherapists hangs out on expectation setting. If you inform a patient that you are going after comfort that enables coughing and walking, not absolutely no pain, you straighten goals and decrease unnecessary escalation. The mounting issues equally as much in a gym as in a ward.
Emergency pain administration in the field
Acute discomfort in prehospital and occasion setups presses time and increases variables. You could be functioning under rainfall, in the middle of crowd sound, or in a confined bathroom. A concentrated pain administration course constructed around emergency situation situations trains behaviors that endure chaos.
Scene safety establishes whether you can do more than stabilize. Splinting and placing occasionally decrease discomfort more than medication in the first five mins, especially for long bone fractures or shoulder dislocations. Inhaled analgesia like methoxyflurane can knock the pain down swiftly while you prepare IV access if procedures enable. Intranasal fentanyl has a function when venous gain access to is difficult, but you need clear application tables and rise requirements. PUAEME008 Provide discomfort administration puts these decisions right into a list structure that teams can debrief reliably after shifts.
Documentation is part of the therapy. I puaeme008 stress a regular handover line to paramedics or ED staff that consists of mechanism, peak discomfort, feature support, treatments with times and dosages, and the first reassessment point. In practice this protects against replicate dosing and keeps the analgesic intend on a sensible track.
Edge cases are entitled to interest. Elderly individuals with renal problems and polypharmacy need conservative application and even more constant observation. Individuals with opioid resistance might need greater preliminary dosages, yet they are just as susceptible to damaging effects if you pile sedatives. Agitated head injury makes complex both evaluation and analgesia choice. Quality discomfort monitoring training courses resolve these without alarmism, offering practical decision trees.
Chronic pain, rehab, and the lengthy game
Chronic pain monitoring is not the main target of every certification program, yet even emergency‑focused programs need to provide you a framework for the person who reappears over and over. A physio therapist who understands central sensitization and anxiety avoidance can assist a mindful person through rated task with specific flare‑up regulations. A registered nurse who clarifies that full pain silence is not the criteria can reset expectations that prevent unneeded admission.
Behaviorally anchored methods make the abstract useful. For example, an individual with chronic reduced pain in the back may devote to 2 walks daily, each just long enough to reach a 3 to 4 out of 10 rise hurting that solves to baseline within 24-hour. This "expose but do not bewilder" principle functions throughout joints and medical diagnoses, and it is teachable in a pain administration certification program with patient scripts and examples.
Building a training plan for your team
In busy solutions, education takes on lineups and budget plans. A blended method is frequently the only feasible path. I have seen the most effective outcomes when organizations blend a foundational discomfort administration program for all medical professionals with targeted modules for specific duties. For brand-new starters, a short certification course in pain management that consists of PUAEME008 offer pain monitoring covers the severe base. For ward registered nurses, a ward‑based workshop on opioid conversions and PCA troubleshooting can minimize phone call to after‑hours doctors. For physio therapists, a two‑day pain neuroscience workshop paired with monitored case speaks with cements skills.
One hospital I dealt with cut post‑operative pain escalations by concerning a quarter over 2 quarters after executing three changes: a standardized review schedule embedded in electronic observation charts, a straightforward nurse‑led path for dental multimodal analgesia within specified ceilings, and a communication script to set client expectations at admission. These modifications expanded from training yet were sustained by process tweaks. Programs begin the change, systems keep it going.
What analysis and certification look like
Pain monitoring accreditation is available in several flavors. Some are formal devices like PUAEME008 with sensible evaluation and circumstance screening. Others are certificate programs used by colleges or expert universities with on the internet components, study, and proctored exams. The reliable ones go beyond several option. Anticipate observed structured medical examinations, drug computation checks, and substitute handovers. For registered nurses and paramedics, local medication authority recommendations or method sign‑offs could ride on the back of the course.
Keep an eye on recency requirements. Skills dull without usage, especially procedural analgesia and gadget usage. Great programs define re‑credentialing cycles, commonly every two to three years, and allow shorter refresher modules instead of duplicating the entire discomfort management certification course.
Selecting a carrier without purchaser's remorse
Marketing language around discomfort administration training is usually shiny. Strip it back with a few practical checks.
- Faculty reliability: instructors with current clinical technique, not simply scholastic titles. Ask just how usually they work at the bedside or in the field. Assessment roughness: a composed examination alone is not enough. Look for simulation, drug computations, and observed functional skills. Protocol placement: products need to match your neighborhood medication formularies and legal frameworks. Imported material without localization wastes time. Post course support: access to updates, fast reference guides, and a line for inquiries during the first months of implementation. Outcome tracking: carriers who aid you measure adjustments, such as decrease in time to first analgesia or improved documents completeness.
These checks normally remove programs that promise a pain monitoring certificate but supply little past slides.
Practical pharmacology, common mistakes, and safer habits
Pain administration training for nurses and paramedics often discloses patterns of over and under‑treatment. Under‑treatment originates from worry of opioids or missing out on non‑drug choices. Over‑treatment hides in stacking sedatives or stopping working to reassess after an initial dose.
I teach a practice loophole that improves safety and security. Dosage modestly within protocol, established a timer for reassessment, check discomfort, sedation, respiration, and function, then make a decision whether to duplicate, switch over agents, or include an adjunct. The feature support is crucial. If a client claims pain is still 6, yet they can now cough, take a sip, and pivot sideways, that might be an acceptable plateau, specifically in the very first hour after a severe injury or major surgery.

Multimodal regimens function when they are really set up and complementary. Paracetamol in a timely manner, an NSAID if not contraindicated, a localized alternative like topical diclofenac or lidocaine spots when appropriate, and regionals or blocks when available. Opioids after that cover optimals as opposed to construct the entire structure. An excellent pain administration program reveals you how to compose these orders, discuss them with prescribers, and spot when a client is getting on adverse effects that need to trigger a switch.
Documentation that improves care, not simply compliance
Documentation often obtains mounted as a conformity task. Suffering administration it is a clinical tool. The mix of a clear standard, a treatment record with times and doses, and a useful target tells the next clinician where to grab. I motivate short however certain access: "Pain 8 at rest, 10 on coughing. Objective: coughing and sit up with pain ≤ 6. Given oxycodone 5 mg 14:05, paracetamol 1 g 14:10, taught cushion splinting. Reconsidered 14:35: pain 5 on coughing, rested at side of bed." That tight note assists the next registered nurse plan and guards the individual from duplicate dosing.
Courses that consist of charting technique, particularly with local digital wellness records, deserve greater than polished concept alone. It is one point to recognize you need to reassess in 20 to thirty minutes, and an additional to see exactly where to log it in your system so the alarm system reminds you.
How physio therapists convert concept to movement
Physiotherapists often come out of pain monitoring training energized but need anchors for real sessions. Utilize one academic minute at the start to mount the day's objective, after that relocate into rated direct exposure with immediate victories. For instance, an individual scared of back flexion could begin with supported hip joint drills to 20 degrees, paired with slow nasal breathing, after that advance to sit‑to‑stands with a cushion. The workout option issues much less than the safety signs and development reasoning. Discomfort neuroscience education and learning without a movement strategy seldom sticks. A pain monitoring certification course that sets quick, repeatable scripts with details progressions is worth the time.
Nurses as planners of the analgesic plan
On surgical wards, nurses usually coordinate the series of analgesia. A strong pain monitoring training for registered nurses describes exactly how to time drugs about physiotherapy, wound treatment, and meals. Giving a short‑acting opioid 20 minutes prior to breast physical rehabilitation can make the difference in between productive coughing and superficial breathing. Similarly, think of evening application to stop 3 a.m. pain spikes that unravel rest and extend the recuperation trajectory. When you see individuals as relocating via a 24‑hour pain rhythm, not simply fixed vitals, your treatment timing improves.
Ethics, equity, and predisposition suffering assessment
Courses appropriately emphasize the technicians of analgesia, however ethics and equity issue just as much. Discomfort is under‑treated in particular populaces due to bias, communication barriers, or presumptions about drug‑seeking. Training needs to emerge these patterns. Usage interpreters early. For individuals with cognitive disability, lean on habits scales and family insights. File plainly when you decline or postpone opioids and what option you used. These routines shield people and clinicians, and they can be taught.
Making your certification count after the course
New abilities discolor if they live only in certificates. Fold what you find out right into daily technique. I ask teams to take on one visible change after a discomfort monitoring program. Instances consist of systematizing a 30‑minute review home window, including function‑based objectives to every emergency pain management analgesia plan, or putting a tiny "analgesia titration aid" card on the medicine trolley. Tiny artifacts maintain the training active and spread it to brand-new colleagues.
Many medical professionals accumulate multiple certifications over an occupation. Pick deepness over volume. A strong pain monitoring accreditation training course, revitalized with targeted updates every number of years, defeats a loads superficial badges.
Where short training courses fit in a lengthy career
Short training courses suffering management fill up the voids between huge career steps. A two‑hour upgrade on intranasal analgesia, an early morning on neuropathic pain screening, a night webinar on opioid conversions, each refines judgment and saves time later. They likewise prepare you for larger actions, such as an official pain monitoring certificate that might qualify you to show peers or lead a solution improvement project.
For paramedics and first responders, a short refresher anchored to PUAEME008 Provide pain monitoring keeps abilities sharp and documents regular across teams. For ward nurses, bite‑sized sessions connected to local instance evaluates keep the web content grounded in reality.
Final thoughts from the floor
Pain administration is technological and human at the same time. The medications, devices, and ranges matter, yet the outcome depends upon what you observe, how you time treatments, and exactly how you explain the strategy. The appropriate discomfort management training program offers you the devices, however your practice transforms them right into alleviation the client can feel.
Choose programs that value your extent, demand genuine analysis, and show how to act under pressure. If you operate in emergency care, a PUAEME008 provide pain monitoring course is a practical anchor. If you practice on wards or in clinics, search for discomfort management certification that ties medicine, activity, and frame of mind together. After that make the training visible in your notes, your conversations, and your routines. That is just how certificates become care.